Anatomy, physiology and pathology of the lacrimal system
Anatomy and Function of the Lacrimal System
The lacrimal system is responsible for the production and drainage of tears from the surface of the eye. It consists of two main components:
- Secretory component – responsible for tear production; it includes the lacrimal gland and accessory glands located in the conjunctiva and eyelids.
- Drainage component – responsible for draining tears from the ocular surface into the nasal cavity; it includes the lacrimal puncta, canaliculi, lacrimal sac, and nasolacrimal duct.
The main lacrimal gland, located in the superolateral part of the orbit, and the accessory glands (Krause, Wolfring, Meibomian, Zeis, and Moll) produce the individual components of the tear film, which serves to protect and hydrate the ocular surface.
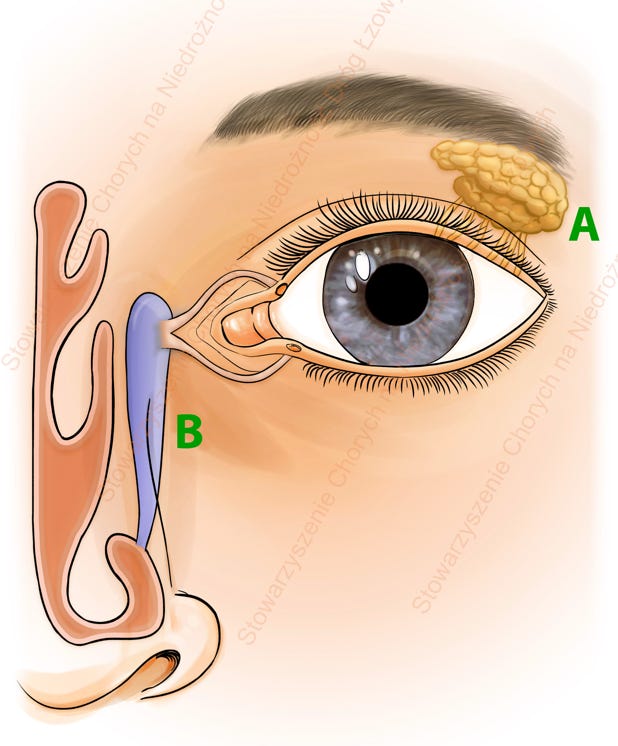
Lacrimal system: A- lacrimal gland; B- lacrimal drainage pathways
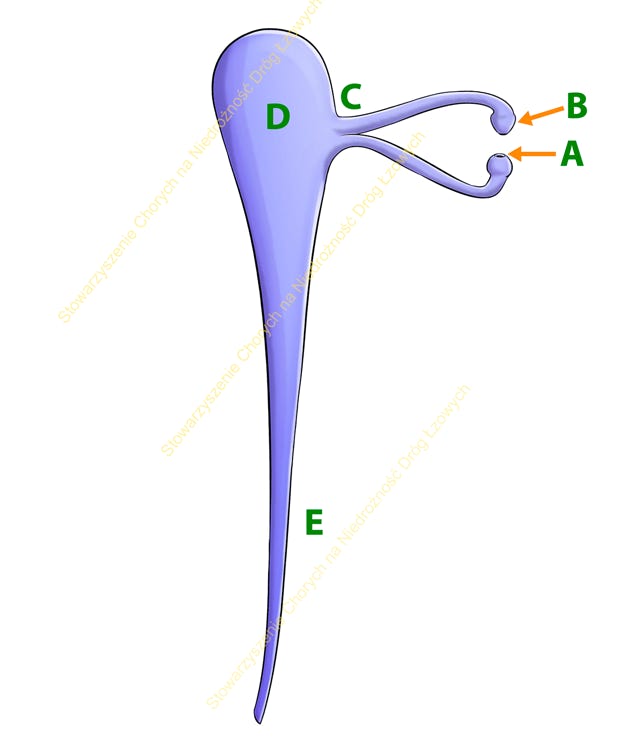
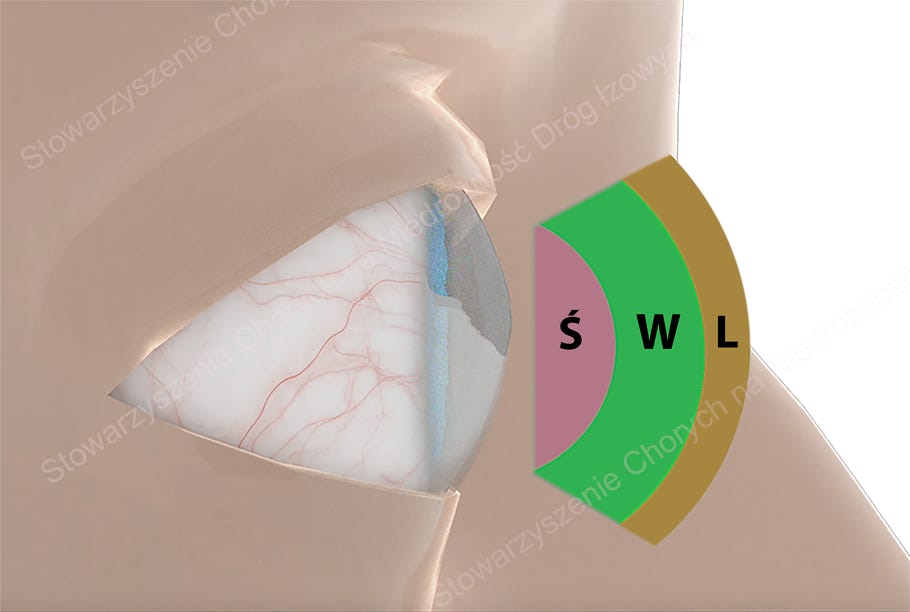
Lacrimal drainage pathways: A- inferior canaliculus; B- superior canaliculus; C- common canaliculus; D- lacrimal sac; E- nasolacrimal duct